
Ghana 2017: Reflections from Team Member Connor Kuipers
By: Connor Kuipers
Flying from Grand Rapids to Washington D.C. the day after the Christmas holiday, I realized that I was about to embark on an adventure that would change many things for me: my knowledge of a completely new culture, my understanding of medicine in general, my confidence in my decision to pursue the practice of medicine, and most importantly my ability to change people’s lives as I counseled and assisted in meeting their medical and surgical needs.
However, in that first hour long flight to D.C. I had no clue that I would learn any of these things, and I had very few expectations for this Ghana mission. Dr. G sufficiently prepared my companions and I for this trip, but he definitely gave few details. In hindsight, this allowed me to be more vulnerable to what the trip had to teach me. Already in the first 30 minutes of the car ride back to Derwood I realized I would be digesting countless “dissertations” on everything from the history and landmarks of the rivers of greater D.C. to filariasis associated with elephantiasis.
Everybody that goes on missions with Dr. G takes part in a tutorial every night that focuses on observations and questions from throughout the day as well as topic presentations from all the members of the mission. This practice, as well as the constant explanations and demonstrations are priceless. The rule of thumb about priceless things is that they can be extremely precious to the receiver or they can be squandered. I hope that these priceless lessons I learned will guide me through my next ten yea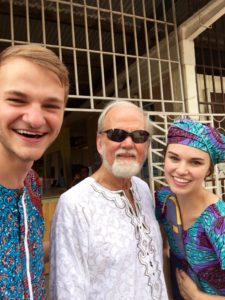 rs of school and then for the rest of my career and life.
rs of school and then for the rest of my career and life.
Mission to Heal has three goals on every mission and I think that these three goals do a good job of outlining my reflections of this trip. The first goal is the most obvious one, and that is to bring medical and surgical care to those who are too sick, too poor, or too far away to reach it. The setting for our mission, Essikado Hospital, was a district hospital that employed only two full time doctors and brought in specialists on certain days and occasions. Notice how I didn’t say it was a small hospital. It served an incredible amount of people for the resources it ad. What it was specifically lacking is what we came to provide, and that is surgical care.
The vast majority of the cases that came into their small Operating Theatre were OB/GYN cases. Scheduled Cesareans were on Wednesdays along with other small cases. For this a part-time doc came in. We rose their three cases and emergencies a week to 7-9 major operations every day. Because of this, our list of major operations (hernia, salivary gland tumor, goiter, hydrocele) completed peaked to above one hundred by time we left. Minor operations (lipoma, fibroma, sebaceous cyst, ganglion cyst) also reached well over one hundred. This means that more than two hundred patients had a semi to very major life change after their operation. When you have a hernia in your scrotum hanging down to your knees for 30 years or a growing thyroid the size of your head that is inhibiting eating and breathing, the improvement in every day life after its treatment is significant. These are all people who would never be able to afford these “elective” operations that are not covered by health care unless we were around.
On top of the surgical care, we provided basic medical care by screening hundreds of patients every day. Many of the cases were general pains all over the body, headaches, foot pain, etc., which can be understood in these women who walk everywhere with fifty plus pounds of merchandise and personal items balanced on their heads. For these patients we had ibuprofen and Tylenol to dull the pain, free of charge, which we would prescribe to them from our pharmacy. Many had high blood pressure that we treated and followed up with instructions to see a local doctor. Malaria is also quite common (all Africans get it at least once) and the headache, varying fever, and chills always received a malaria test and eventually a three-day dosage of malaria medication.
Lastly, of course, there were our surgical cases which we caught and scheduled as well as we could. This provided a huge problem after the first week. We would see double the hernias in a day in screening than we were able to operate on. Logically, those waiting patient numbers compound after a week and explode after three. One of Dr. G’s famous lines is, “They all think they will be the last one before we leave.” And it was true! They heard from the radio or their neighbor or church or second cousin that we were here doing operations FOR FREE! There was no mention of a departure date or the fact that we would only have time to do less than half that we screened. I know this was a hard realization for me and some of the other volunteers to make. We couldn’t fix all of Essikado or Ghana or Africa.
Mission to Heal: Pillar 1
Provide surgical operations and medical care to those who need it, who have limited or no access to it, and who cannot afford it.
As far as the first goal of Mission to Heal goes, we had good numbers and provided health care for a ton of good people who wouldn’t have received it otherwise. Did we help even a fraction of the people? Of course not. If this is where Mission to Heal goals ended I would be a little depressed here sitting on my transatlantic flight home. But it’s not! And with that knowledge that we accomplished other goals I can be thrilled with the fact that we helped so many individuals. I had many special people come up to me and give all their thanks, prayers, and God’s blessing.
I was sitting with someone during a hernia operation under local anesthetic, (a.k.a. he could feel e verything going on inside his body besides for the initial skin incision) and he was in a ton of pain. After waiting in the heat for four days to get this operation and now having his insides pulled and ripped he was thanking me and praising God for me in many languages (including Spanish, which was very unique and exciting for me). Although there were many people that hated me for making them wait everyday for a week for an operation that “we might have time to do” and that they felt very entitled to, there were others that told me how thankful they were that I sat down with them, called them by name, and listened to their problem no matter how insignificant it was. This was beneficial for the patient and me, which is why I feel like it is a good use of my time in the future.
verything going on inside his body besides for the initial skin incision) and he was in a ton of pain. After waiting in the heat for four days to get this operation and now having his insides pulled and ripped he was thanking me and praising God for me in many languages (including Spanish, which was very unique and exciting for me). Although there were many people that hated me for making them wait everyday for a week for an operation that “we might have time to do” and that they felt very entitled to, there were others that told me how thankful they were that I sat down with them, called them by name, and listened to their problem no matter how insignificant it was. This was beneficial for the patient and me, which is why I feel like it is a good use of my time in the future.
Mission to Heal: Pillar 2
Equip medical professionals with the heart and hands to function in needy and poorly-resourced conditions.
The second pillar of Mission to Heal is the teaching that goes on within the mission group. A lot of this comes straight from Dr. G but quite a bit comes from the presentations I would give and that I would hear. My first topic was hernias, which were arguably the most important thing to learn the cause of, how to identify, and how to treat right away. One of my other topics was Spinal Diseases, specifically in Pediatrics, which was chosen for me because of my interest in working with kids some day. We give our presentations with Dr. G’s help, but even more helpful was a patient showing up the next day with the exact problem that you had a presentation on. It would happen that there was a talk about filariasis and a case of elephantiasis showed up, or an explanation of the symptom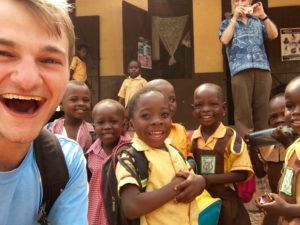 s of a migraine and a patient the following morning would list off the exact same symptoms as were described. I am a completely visual learner, so this was perfect for me to solidify the information in my mind. Dr. G would joke that we should be paying tuition, and I agreed! I easily grew my medical knowledge tenfold on this trip. The direct application is priceless and it is exactly what that second goal of Mission to Heal is all about. I learned so much through this trip, but even more importantly I am beginning to comprehend how much more there is to learn and how excited I am to learn about it. It most definitely solidifies my drive to become a physician.
s of a migraine and a patient the following morning would list off the exact same symptoms as were described. I am a completely visual learner, so this was perfect for me to solidify the information in my mind. Dr. G would joke that we should be paying tuition, and I agreed! I easily grew my medical knowledge tenfold on this trip. The direct application is priceless and it is exactly what that second goal of Mission to Heal is all about. I learned so much through this trip, but even more importantly I am beginning to comprehend how much more there is to learn and how excited I am to learn about it. It most definitely solidifies my drive to become a physician.
Mission to Heal: Pillar 3
Equip locals to provide the medical care so that the community attains a greater degree of self-sufficiency.
The last pillar of Mission to Heal is arguably the most important and definitely the most difficult. As I mentioned before, providing health care for a thousand people is honorable and life changing but it is also miniscule when you consider the 2.4 million people living in just the Western Region of Ghana. Leaving behind skills which Ghanaians can use to help anyone in need of health care in the Western Region is what we were really striving to do. This was very difficult on this mission. We were in an operating room with staff that were very content in their surgical ability with the maternity needs that came in and the two doctors in the hospital had little interest in adding more onto their plate. And I don’t blame them! This is why we were able to take advantage of many “political” opportunities which brought Dr. G closer to different surgeons at the regional and university hospitals where he will be able to pass on his skills, or with the Minister of Health who has a large influence over future possibilities for missions, and even with businessmen who would be able to fund the dream of having a Mobile Surgical Unit come in through Ghana. Although I have not seen the MSU in action, I can see why Dr. G believes it is the perfect tool to allow the three goals of every Mission to Heal mission to come together perfectly.
G closer to different surgeons at the regional and university hospitals where he will be able to pass on his skills, or with the Minister of Health who has a large influence over future possibilities for missions, and even with businessmen who would be able to fund the dream of having a Mobile Surgical Unit come in through Ghana. Although I have not seen the MSU in action, I can see why Dr. G believes it is the perfect tool to allow the three goals of every Mission to Heal mission to come together perfectly.
The vision of the MSU in Western Africa excites me so much. I was forced to see so many times how a three bed unit that allowed for a quick turnover of patients would be much more practical than a one bed operating room that was shared with maternity. This is for three reasons: five times more patients helped, space to teach anyone willing to learn, and opportunity for many volunteers to come and share their skills with those willing to learn. This is the future of surgical missions in countries that have need and I am so thrilled to have been a part of it, and yes, continue to be a part of it.
To conclude my reflection, I am happy to come to the realization that this is not the end of the road for me. I am too invested into what is happening through Dr. G and too eager to learn more from someone with 50 years of experience with patients. I am too excited about a possibility to improve patient outcomes and numbers of patients reached with a Mobile Surgical Unit. Most importantly, I am too overwhelmed by the need for basic health care in an otherwise stable area where morbidity and mortality from basic and treatable diseases and accidents ruins and shortens lives every day. I am honored to have been a part of it and I am thrilled to find my place in the mission again as soon as I can.